Some days, nothing is wrong—but nothing feels right either.
You’re sober. Life is mostly okay. But the fire’s gone quiet.
You’re not in danger of relapse. But you’re also not quite living the way you imagined when you first got clean. It’s like the colors faded. You’re here—but not fully here.
If that’s where you are, you’re not alone. This stretch of recovery doesn’t get talked about enough. It’s not early chaos. It’s not relapse crisis. It’s something quieter. And it can be just as disorienting.
But here’s what I want you to know: the tools you built in opiate addiction treatment weren’t just for emergencies. They were for now, too—for the still, strange middle. The part where healing keeps going, even when no one else can see it.
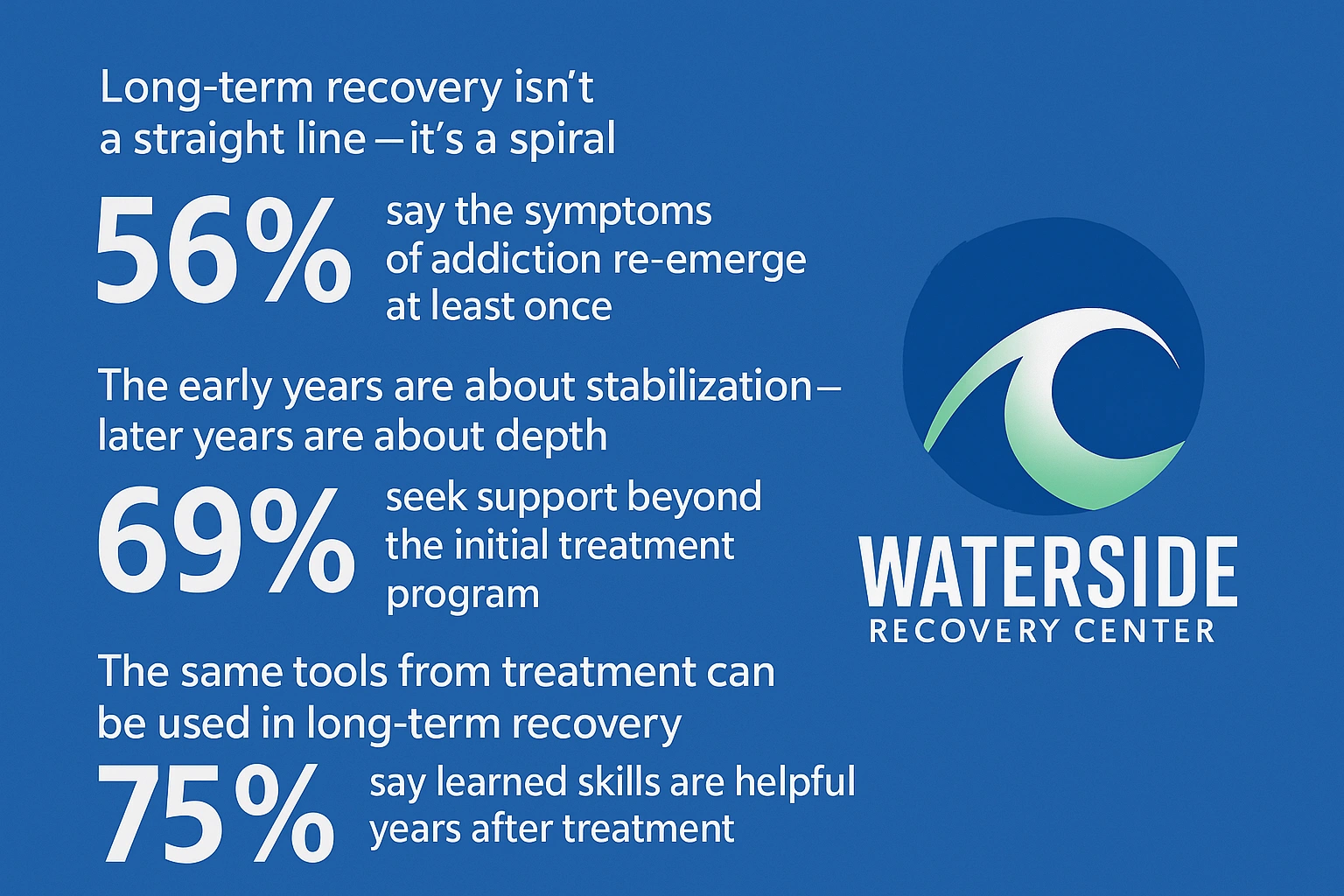
Long-Term Recovery Isn’t a Straight Line—It’s a Spiral
You don’t wake up ten years sober and feel “done.” Recovery isn’t graduation. It’s growth—and growth isn’t always linear.
Some parts repeat:
You might revisit old grief in a new way.
You might realize a behavior you thought was “just a quirk” is still a leftover survival mechanism.
You might get tired. Spiritually tired. Emotionally worn out.
That doesn’t mean you’re doing it wrong. It means you’re still healing.
The early years of sobriety are about stabilization—detox, routine, structure, learning to live without.
But the later years? They’re about depth.
Opiate Addiction Treatment Was More Than Just a Starting Point
When I first stepped into treatment, I thought it was just about stopping the pills.
But what I really gained was a new way to live.
Boundaries.
Emotional language.
A community where people spoke truth—without performance.
It was in those group rooms that I learned I could say things like, “I feel disconnected,” and not be met with panic or dismissal.
I didn’t know back then how often I’d need to use those same skills years down the line—on regular days when everything looked fine, but nothing felt aligned.
That’s the thing no one tells you:
The further into recovery you go, the subtler the symptoms—and the more important the tools.
You’re Allowed to Miss Something You Can’t Name
Some people call it spiritual flatness.
Others describe it as numbness, restlessness, or “the blahs.”
It’s that weird space where life has become functional but not full. You’re working. Sleeping. Eating. But something inside feels off.
And because it’s not urgent or dangerous, it’s easy to ignore.
You might hear yourself say:
- “I should be grateful.”
- “Other people have it worse.”
- “At least I’m not using.”
But healing isn’t just about surviving. It’s about returning—to yourself, to meaning, to feeling fully alive.
You’re allowed to miss that aliveness. And you’re allowed to seek it again.
Your Recovery Still Counts—Even When It Feels Flat
Let’s be real: not every season of sobriety feels inspiring.
Some days are just… maintenance. Some months, even.
And if you’re in that space now—where things are steady but dull—that doesn’t erase the work you’ve done. It doesn’t mean you’re regressing. It just means you’ve reached a layer of healing that asks for a different kind of attention.
Early on, success looked like not using.
Later, it looks like telling the truth even when you’re tired.
It looks like reaching out before things get urgent.
It looks like choosing growth even when no one’s watching.
This stretch of recovery is quiet—but it’s sacred.
The Same Tools Work—You Just Use Them Differently
Remember when you learned to:
- Pause before reacting
- Name the feeling instead of the behavior
- Let someone else hold space when you couldn’t hold yourself?
Those aren’t early recovery tricks. They’re lifelong tools.
You don’t need a crisis to revisit a group room. You don’t need to relapse to talk to a counselor. You don’t have to hit a low to ask for more connection.
Your opiate addiction treatment taught you how to return to yourself. You can do that as many times as you need.
In fact, the willingness to return? That is the sign of continued recovery.
You Don’t Have to Do This Part Alone
Here’s what I’ve seen over the years:
Some of the strongest people in recovery hit this wall. Not because they’re weak—but because they’ve been strong for so long, they forgot what it feels like to rest in support.
If that’s you—if you’re reading this and thinking, “Maybe I am carrying more than I realize”—you’re already halfway there.
You don’t have to sort it all out in your head.
You don’t have to figure out what you need before you ask for help.
You just have to start talking again.
If you’re in Kingston, Duxbury, Marshfield or anywhere in Plymouth County, MA, Waterside Recovery is still here for you. We’ve never stopped seeing you.
What Does “Returning” Look Like?
For some, it means checking in with a former counselor.
For others, it’s rejoining a group—or just visiting once.
For some, it’s a fresh round of outpatient care tailored to where they are now.
There’s no shame in continuing care.
There’s wisdom in knowing when you’re ready for another layer of growth.
Maybe the part of you that’s feeling stuck isn’t failing—it’s inviting you to heal something deeper.
Recovery Isn’t Just About Avoiding Pain. It’s About Reclaiming Joy.
When’s the last time you laughed so hard your stomach hurt?
When’s the last time you cried without apologizing for it?
When’s the last time you looked in the mirror and saw someone fully alive?
You deserve that version of recovery. Not just the quiet survival—but the soulful kind. The kind that lets you breathe deeper and feel again.
That’s what long-term recovery can offer, if you’re willing to come back—not because you have to, but because you want more than flatness.
FAQs: Long-Term Sobriety and Staying Emotionally Well
Is it normal to feel disconnected even after years of recovery?
Yes. Many people in long-term recovery experience emotional flatness, spiritual dryness, or subtle dissatisfaction. This doesn’t mean your recovery is failing. It means it’s evolving—and it may be time to reconnect with deeper support.
What if I don’t feel like I’m in “crisis”—but I still need something?
You don’t need a crisis to deserve care. Returning to therapy, group work, or even just open conversation can be valuable maintenance—not a step backward.
Can I return to treatment if I haven’t relapsed?
Absolutely. Many alumni return for check-ins, therapy tune-ups, or to explore unresolved emotional or relational patterns. At Waterside Recovery Center, we support growth at every stage—not just the beginning.
I’m in a different season of life now. Will the support still apply?
Yes. Whether you’re managing new responsibilities, grief, relationships, or just emotional fatigue, the core principles of recovery—honesty, connection, boundaries, reflection—apply in every chapter.
I live nearby—do I have to travel far to get help?
Not at all. Waterside Recovery offers support for clients in Plymouth County and surrounding regions like Bristol County, MA. You don’t need to leave your life behind to get back in touch with yourself.
You’re Still Here. And That Still Matters.
Your sobriety isn’t a past achievement. It’s a living thing.
It deserves care. Nourishment. Reconnection.
If you’re ready to explore what healing looks like now—not just back then—we’re here for that conversation.
Call (866)671-8620 to learn more about our Opiate Addiction Treatment services in Plymouth County, MA.
You’re not lost. You’re just being invited deeper.
Let’s walk that road together.