Maybe you’ve been in treatment before. Maybe you stayed for a little while, or maybe you ghosted after a few sessions. Either way, you’ve probably wondered: was it me? Or was the program just… not the right fit?
At Waterside Recovery’s outpatient treatment program, we hear it all the time—people thinking they “failed” at treatment, when really, the program didn’t match what they needed. The truth is simple: no single therapy works for everyone. You’re allowed to choose options that actually make sense for you.
This blog walks you through how to pick therapies that work with your brain, your patterns, and your life. Not every therapy is your therapy—and that’s completely okay.
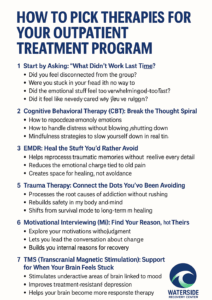
1. Start by Asking: “What Didn’t Work Last Time?”
Before you jump into lists of therapy options, take a second to reflect:
- Did you feel disconnected from the group?
- Were you stuck in your head with no way to stop spiraling?
- Did the emotional stuff feel too overwhelming too fast?
- Did it feel like nobody cared why you were struggling?
It’s okay to admit that certain approaches didn’t click. Getting honest about those gaps helps you find therapies that target the right areas, instead of repeating the same frustrating cycle.
2. Cognitive Behavioral Therapy (CBT): Break the Thought Spiral
If you’ve found yourself stuck in negative self-talk—constantly beating yourself up or assuming the worst—CBT might be your anchor.
CBT focuses on:
- Spotting distorted thought patterns.
- Replacing automatic negativity with more balanced thinking.
- Building concrete tools to interrupt spiraling moments.
This therapy is helpful when your own thoughts feel like the enemy. It offers structure and logic in moments when your brain tries to talk you into self-destruction.
3. Dialectical Behavior Therapy (DBT): Survive the Emotional Whiplash
Some people don’t struggle with thoughts as much as feelings—those intense, hard-to-control waves of emotion. DBT is built for this.
DBT teaches you:
- How to regulate overwhelming emotions.
- How to handle distress without blowing up or shutting down.
- Mindfulness strategies to slow yourself down in real time.
If you’ve left treatment before because the feelings got too big too fast, DBT shows you how to survive the storm without losing yourself in it.
4. EMDR: Heal the Stuff You’d Rather Avoid
Sometimes, what sabotages outpatient treatment is the weight of old trauma. You show up, but the old stuff drags you down, making it hard to focus on today’s recovery.
That’s where EMDR (Eye Movement Desensitization and Reprocessing) comes in:
- It helps reprocess traumatic memories without needing to relive every detail.
- You reduce the emotional charge tied to old pain.
- You create space for healing, not avoidance.
At Waterside Recovery, EMDR is available for clients whose past keeps hijacking their present—because no one heals while trapped in old wounds.
5. Trauma Therapy: Connect the Dots You’ve Been Avoiding
Not everyone is ready for EMDR. Some people need to work through trauma more slowly, with words, trust, and gradual exposure. Trauma therapy helps:
- Process the root causes of addiction without rushing.
- Rebuild safety in your body and mind.
- Shift from survival mode to long-term healing.
For many who’ve ghosted treatment, trauma therapy makes the difference—it answers the “why” behind destructive patterns that felt impossible to change before.
6. Motivational Interviewing (MI): Find Your Reason, Not Theirs
Sometimes you leave treatment because you’re not sure you really want to quit. You’re not sold on sobriety. You’re half-in, half-out. That’s where Motivational Interviewing can change the game.
MI focuses on:
- Exploring your motivations without judgment.
- Letting you lead the conversation about change.
- Building your internal reasons for recovery—not just doing it because someone else says you should.
It’s permission to be unsure—while still getting help. No lectures. Just honest dialogue.
7. TMS (Transcranial Magnetic Stimulation): Support for When Your Brain Feels Stuck
Sometimes, the problem isn’t therapy—it’s your brain chemistry. TMS offers a non-invasive option for people stuck in cycles of depression and foggy thinking, especially when talk therapy hasn’t been enough.
TMS helps:
- Stimulate underactive areas of your brain linked to mood.
- Improve treatment-resistant depression.
- Help your brain become more responsive to therapy.
If you’ve felt like therapy just couldn’t get through to you, TMS might help clear the static.
8. You’re Not “Bad at Treatment”—You Just Needed Options
Dropping out of treatment doesn’t mean you’re hopeless. It means you didn’t have the right fit, the right timing, or the right support. That’s fixable.
At Waterside Recovery’s outpatient treatment program in Plymouth County, MA, we don’t just offer one therapy style. We help you figure out what’s actually working—and adjust along the way.
You’re allowed to want a program that makes sense for your story, not just a generic checklist.
Frequently Asked Questions (FAQs)
Is it normal to leave treatment and come back?
Yes—very normal. Many people take more than one attempt to find their footing in recovery. What matters isn’t how many times you step away—it’s that you come back when you’re ready to try again.
What if I don’t know which therapy is right for me?
That’s okay. A good outpatient program will help you figure that out through clinical assessments, conversations about your needs, and trying different approaches. You’re not expected to know all the answers on day one.
Can I mix different therapies in outpatient care?
Absolutely. Most successful treatment plans combine several approaches. For example, you might do CBT and trauma therapy, or DBT alongside motivational interviewing. Therapy is adjustable—not one-size-fits-all.
Does outpatient treatment include medication support?
Yes. Medication can be part of outpatient treatment when needed—whether it’s for cravings, mood stabilization, or managing anxiety or depression. Your clinical team can guide you through options like MAT (medication-assisted treatment) or TMS if it’s appropriate.
What if I have a job or family responsibilities?
Outpatient programs like ours are designed to work around your life. Many people balance outpatient care with work, school, or family—especially with flexible daytime or evening options.
You Don’t Have to Get It Right the First Time—You Just Have to Keep Going
Trying again doesn’t make you weak. It makes you brave. It means you’re willing to figure out what actually helps you feel better, instead of settling for survival mode.
Call (866)671-8620 to learn more about our outpatient treatment program services in Plymouth County, MA. Let’s make your next try feel different—because this time, it will be.